Signs Your Gut Fungus May Be Affecting Your Health
Have you ever felt bloated after meals, struggled with ongoing fatigue, or noticed your digestion just isn’t right despite eating well?
Many people live with ongoing digestive discomfort, low energy, or vague symptoms that seem hard to explain. You might feel bloated after meals, notice changes in your mood, or struggle with recurring issues that never fully resolve.
These experiences can be frustrating, especially when routine checkups don’t point to a clear cause.
Over time, it’s natural to wonder whether something deeper such as an imbalance in your gut could be playing a role.
Why Ongoing Digestive Symptoms Can Be Hard to Explain
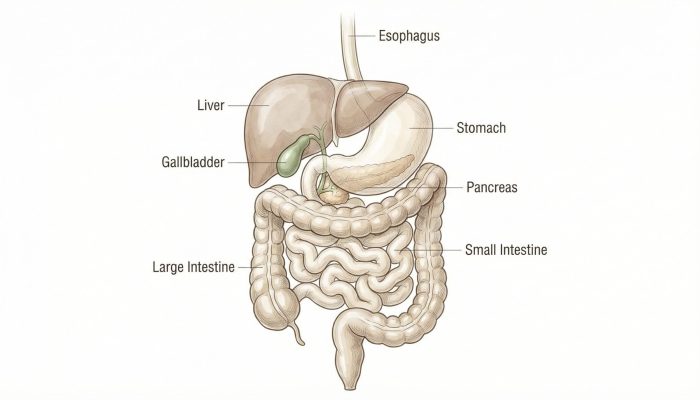
Conversations around gut health have become more common in recent years, and for good reason. The digestive system influences far more than just how food is processed.
Among the many factors that can affect gut balance, fungal overgrowth is one topic that often raises questions and confusion. Understanding how it may show up in daily life can help you make sense of your symptoms and know when to seek professional guidance.
What Gut Fungus and Fungal Imbalance Mean for Digestive Health
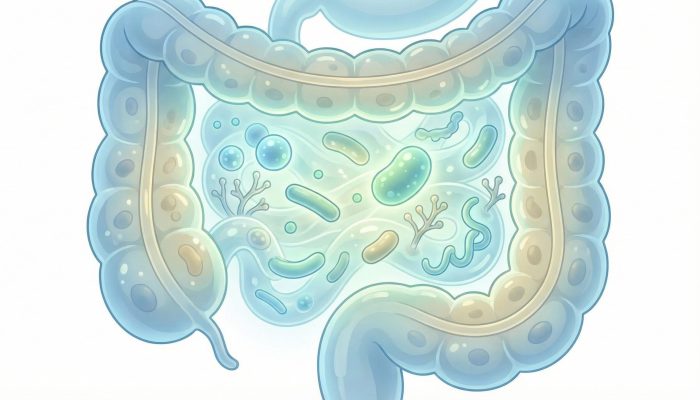
The human gut is home to trillions of microorganisms, including bacteria, viruses, and fungi. In a healthy system, these organisms exist in balance and support normal digestion, immune function, and nutrient absorption. Fungi such as Candida species are a natural part of this environment.
Problems may arise when certain fungi grow more than usual and disrupt that balance. This situation is often referred to as “gut fungal overgrowth.” It does not mean that fungi are always harmful; rather, it suggests that the overall ecosystem of the gut may be out of balance.
This imbalance can sometimes influence how the digestive system and other parts of the body function.
It’s important to note that gut fungal overgrowth is not a single, clearly defined diagnosis. Instead, it is a concept used to describe a potential contributor to a range of symptoms that overlap with many other digestive and metabolic issues.
Why Gut Fungal Balance Matters for Overall Health
The gut plays a central role in everyday health. It helps break down food, absorb nutrients, and communicate with the immune system. It also interacts with the nervous system through what is often called the “gut-brain connection.”
When the gut environment is disrupted, people may notice changes beyond digestion. Energy levels, focus, skin health, and even mood can be affected. While fungal imbalance is only one of many possible factors, it has gained attention because of its potential links to inflammation and immune responses.
Understanding this topic matters because it encourages a broader view of health. Instead of focusing only on isolated symptoms, it highlights how different systems in the body are connected and why persistent, unexplained symptoms deserve careful evaluation.
Common Signs Your Gut Fungus May Be Affecting Your Body
Symptoms linked to gut fungal imbalance can vary widely from person to person. They also overlap with many other conditions, which is why self-diagnosis is not recommended. Commonly reported signs include:
1. Ongoing Bloating or Gas
Some people notice frequent abdominal discomfort, especially after meals.
2. Changes in Bowel Habits
This may include diarrhea, constipation, or alternating patterns without a clear trigger.
3. Unexplained Fatigue
Feeling tired despite adequate sleep can sometimes be associated with digestive imbalance.
4. Sugar or Carbohydrate Cravings
Strong cravings may be reported, though they can have many causes.
5. Brain Fog or Trouble Concentrating
Difficulty focusing or feeling mentally “cloudy” is a common but non-specific complaint.
6. Skin Issues
Rashes, itching, or flare-ups of existing skin conditions may coincide with gut concerns.
7. Mood Changes
Irritability, low mood, or anxiety can sometimes accompany digestive symptoms.
Important note: These symptoms are non-specific and can be linked to many medical or lifestyle factors. Having one or more of them does not mean you have a fungal overgrowth.

Possible Causes of Gut Fungal Imbalance
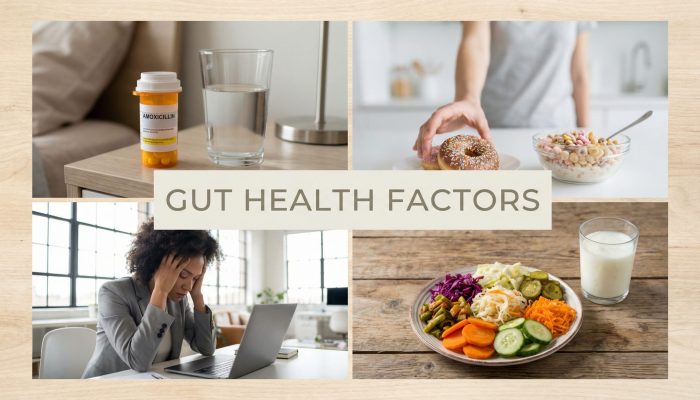
Several factors may contribute to changes in the gut’s fungal balance. Often, it is not one single cause but a combination of influences over time.
1. Frequent or Recent Antibiotic use
Antibiotics can reduce beneficial bacteria, which may allow fungi to grow more easily.
2. Diets high in Added Sugars and Refined Carbohydrates
Certain fungi thrive on simple sugars, though diet alone does not determine gut balance.
3. Chronic stress
Ongoing stress can affect digestion, immune function, and gut motility.
4. Underlying health conditions
Conditions that affect immunity or digestion may influence the gut environment.
5. Hormonal changes
Shifts related to pregnancy, menopause, or certain medications may play a role.
These factors do not guarantee a problem, but they may increase susceptibility in some individuals.
Common Myths About Gut Fungus and Digestive Health
There is a great deal of misinformation surrounding gut fungi. Clarifying common myths can help reduce unnecessary worry.
“All fungi in the gut are bad”
In reality, fungi are a normal part of the microbiome and often coexist harmlessly.
“Gut fungus explains all unexplained symptoms”
Digestive and systemic symptoms are complex and rarely have a single cause.
“You can diagnose this on your own”
Symptoms overlap with many conditions, making professional evaluation essential.
“Eliminating certain foods will fix everything”
While diet matters, no single food plan works for everyone.
Approaching the topic with balance and skepticism can protect against oversimplified conclusions.
How Gut Fungal Imbalance Is Commonly Evaluated
In healthcare settings, concerns about gut imbalance are usually addressed through a broader evaluation of digestive health. This may include:
– Reviewing medical history and medications
– Discussing diet, stress, and lifestyle factors
– Assessing symptoms and their duration
– Ordering tests when clinically appropriate to rule out other conditions
Lifestyle and dietary adjustments are often discussed as part of general digestive support. In some cases, referral to a gastroenterologist or other specialist may be recommended.
Importantly, approaches vary depending on the individual’s overall health and risk factors.
What Research Suggests About Gut Fungus and the Microbiome
Scientific interest in the gut microbiome has grown rapidly. Research suggests that balance among gut organisms—bacteria, fungi, and others is important for maintaining normal immune and metabolic function.
Studies have explored links between microbiome imbalance and inflammation, digestive disorders, and immune responses. Fungi are increasingly recognized as part of this complex system, sometimes referred to as the “mycobiome.” However, this area of research is still evolving.
Current science does not support simple explanations or universal solutions. Instead, it emphasizes individualized care, careful interpretation of symptoms, and the need for more high-quality research.
Everyday Habits That May Support Gut Health Naturally
While avoiding treatment claims, there are general, supportive habits that may help promote overall gut health:
– Eat a varied, balanced diet
Including a range of whole foods supports diverse gut microorganisms.
– Limit excessive added sugars
Moderation is generally recommended for overall health.
– Manage stress
Techniques such as regular physical activity, relaxation practices, or adequate sleep can support digestion.
– Stay hydrated
Adequate fluid intake supports normal digestive function.
– Pay attention to patterns
Keeping track of symptoms and triggers can be helpful when talking with a healthcare professional.
These steps are not treatments, but they align with widely accepted health guidance.

What to Expect Over Time When Addressing Gut Health Concerns
Gut-related concerns often change gradually rather than overnight. If symptoms are linked to lifestyle or dietary patterns, improvements may take weeks or months. Progress is rarely linear, and occasional setbacks are common.
Patience and consistency are important. Paying attention to overall well-being not just one symptom can provide a clearer picture of what is helping and what is not.
When to Talk to a Healthcare Professional About Gut Symptoms
It is important to consult a qualified healthcare professional if you experience:
– Persistent or worsening digestive symptoms
– Unexplained weight loss or fatigue
– Blood in stool, severe pain, or ongoing diarrhea
– Symptoms that interfere with daily life or mental health
A healthcare provider can help rule out serious conditions, provide appropriate testing if needed, and guide next steps safely.

Key Takeaways on Gut Fungus and Digestive Health
Gut fungal imbalance is a topic that often raises concern, but it is best understood as one possible piece of a larger health picture.
The gut contains a complex community of organisms that usually work together to support digestion and immunity. When balance is disrupted, some people may notice digestive, energy, or mood-related changes.
Symptoms are non-specific and overlap with many other conditions, making professional evaluation essential. A balanced, evidence-informed approach focused on overall gut health, lifestyle habits, and medical guidance—offers the most reliable path forward.
You May Also Want to Read
Recent Posts
Frequently Asked Questions
1. What are the common signs of gut fungal imbalance?
Commonly reported signs may include ongoing bloating, changes in bowel habits, fatigue, brain fog, skin irritation, and sugar cravings. However, these symptoms are non-specific and can overlap with many other digestive or metabolic conditions. A healthcare professional can help determine the underlying cause.
2. Is gut fungus the same as a Candida infection?
Not exactly. Candida is a type of fungus that naturally lives in the digestive tract. In some cases, it can grow more than usual and contribute to imbalance. However, not all digestive symptoms are related to Candida, and proper evaluation is important before drawing conclusions.
3. Can gut fungus affect overall health?
Research suggests that the balance of bacteria and fungi in the gut may influence digestion, immune function, and inflammation. When that balance is disrupted, some people may notice broader symptoms. However, more research is still evolving in this area.
4. What causes fungal overgrowth in the gut?
Several factors may contribute, including frequent antibiotic use, high intake of refined sugars, chronic stress, hormonal changes, or certain medical conditions. Often, it is a combination of influences rather than a single cause.
5. How is gut fungal imbalance diagnosed?
There is no single standard test used in routine practice for general “gut fungal imbalance.” Healthcare providers typically review symptoms, medical history, and may rule out other digestive conditions before considering additional testing when appropriate.
6. Can diet affect gut fungal balance?
Diet plays a role in overall gut health. Diets high in added sugars and highly processed foods may influence microbial balance, while a varied diet rich in fiber and whole foods may support digestive health. Individual responses can vary.
7. Are gut fungus symptoms permanent?
In many cases, digestive symptoms fluctuate over time. If they are linked to lifestyle factors, gradual improvement may occur with supportive changes. Persistent or worsening symptoms should be evaluated by a healthcare professional.
8. When should I see a doctor about gut symptoms?
You should consult a healthcare provider if you experience severe abdominal pain, unexplained weight loss, blood in stool, persistent diarrhea, ongoing fatigue, or symptoms that interfere with daily life. Professional guidance helps ensure safe and appropriate care.
9. Is gut fungal imbalance a recognized medical condition?
Fungi are a normal part of the gut microbiome. While fungal overgrowth can occur in certain medical contexts, the broader concept of “gut fungal imbalance” is still an evolving area of research. A personalized medical evaluation is important for accurate understanding.
10. Can stress impact gut health?
Yes. Chronic stress may affect digestion, gut motility, and the gut-brain connection. Managing stress through healthy lifestyle habits may support overall digestive well-being.